Diagnosis, Evaluation, and Treatment of Adenomyosis.pdf
Adenomyosis, a gynecologic condition characterized by the presence of endometrial glands and stroma within the myometrium, can significantly reduce quality of life. The true prevalence of adenomyosis is unknown. Adenomyosis occurs in 8.8% to 61.5% of women under going hysterectomy, and rates vary widely by differences in diagnostic criteria and variations between and within pathologists. The prevalence is estimated to range from 20% to 34%, based on patients referred for pelvic imaging rather than the general population of women.
子宫腺肌病,以子宫内膜腺体和子宫肌层间质为特征的妇科疾病,可显着降低生活质量。子宫腺肌病的真实患病率尚不清楚。子宫腺肌病发生在 8.8% 至 61.5% 的接受子宫切除术的女性中,发病率因诊断标准的差异以及病理学家之间和内部的差异而有很大差异。根据转诊进行盆腔成像的患者而非一般女性人群,估计患病率在 20% 至 34% 之间。
Heavy menstrual bleeding and dysmenorrhea are commonly reported by women with ultrasonography-confirmed adenomyosis. Adenomyosis is associated with dyspareunia, chronic pelvic pain, infertility, and obstetrical complications, such as preterm birth, smallfor gestational age size in neonates, and preeclampsia. However, it is challenging to attribute symptoms or determine the natural history of adenomyosis because it frequently coexists with other gynecologic disorders, such as fibroids, endometriosis, and endometrial polyps. Because these other conditionsmay be diagnosed more frequently with imaging or surgery, women affected by adenomyosis may learn of their diagnosis only after having symptoms for such long periods of time that they elect to undergo a hysterectomy.
经超声检查确诊为子宫腺肌病的女性通常会报告大量月经出血和痛经。子宫腺肌症与性交痛、慢性盆腔痛、不孕症和产科并发症有关,例如早产、小于胎龄儿和先兆子痫。然而,由于子宫腺肌病常与其他妇科疾病共存,如子宫肌瘤、子宫内膜异位症和子宫内膜息肉,因此很难确定其症状或确定其自然病程。因为这些其他疾病可能会更频繁地通过影像学或手术诊断出来,所以受子宫腺肌病影响的女性可能只有在出现症状很长一段时间后才知道他们的诊断,以至于她们选择接受子宫切除术。
The pathogenesis of adenomyosis is unproven, but evidence supports a role for invagination of the endometrial basalis into the myometrium. Alternatively, metaplasia of displaced embryonic müllerian remnants or differentiation of adult endometrial progenitor cells may be the underlying cause.
子宫腺肌病的发病机制尚未得到证实,但有证据支持子宫内膜基底向子宫肌层内陷的作用。或者,移位的胚胎苗勒氏管残余物的化生或成人子宫内膜祖细胞的分化可能是根本原因。
Diagnosis
诊断
The diagnosis of adenomyosis may be established with a combination of physical examination, imaging, pathology, and (less frequently) hysteroscopy. Typically, bimanual pelvic examination findings reveal a diffusely enlarged “boggy” or soft uterus, which may be mildly tender. The histologic diagnosis of adenomyosis is based on the presence of irregularly shaped islands of endometrial glands and stroma in the myometrium, leading some to term adenomyosis endometriosis of the myometrium or endometriosis interna. The adenomyotic lesions are surrounded by hypertrophic and hyperplastic endometrium, further enlarging the uterus, although uteri rarely exceed 280 g or the equivalent of a 12-week size gravid uterus. Lesions may be dispersed throughout the myometrium or form focal masses, referred to as adenomyoma, leading to potential confusion with fibroids. On gross appearance, adenomyoma, unlike fibroids, lack a well-demarcated border and may have areas of brown staining secondary to hemosiderin deposits. Consensus is currently lacking on other criteria, such as the distance of glands from the basal layer of the endometrium, required for pathologic diagnosis. In addition, diagnoses are increasingly being made based on hysteroscopic observation of endometrial defects, hypervascularization, or submucosal hemorrhagic cysts. There are no laboratory tests diagnostic for adenomyosis, although hemoglobinmay be measured if anemia from heavy bleeding is suspected.
子宫腺肌病的诊断可以通过体格检查、影像学、病理学和(较少见的)宫腔镜检查来确定。通常,双手盆腔检查结果显示弥漫性增大的“沼泽”或柔软的子宫,可能有轻微的触痛。子宫腺肌病的组织学诊断是基于子宫内膜腺体和间质在子宫肌层中存在不规则形状的岛状物,导致一些人将子宫内膜异位症称为子宫内膜异位症或子宫内膜异位症。子宫腺肌病病变被肥厚和增生的子宫内膜包围,进一步扩大了子宫,尽管子宫很少超过 280 g 或相当于 12 周大小的妊娠子宫。病变可能分散在整个子宫肌层或形成局灶性肿块,称为腺肌瘤,导致可能与肌瘤混淆。从大体上看,腺肌瘤与肌瘤不同,边界不清,可能有继发于含铁血黄素沉积的棕色染色区域。目前尚缺乏其他标准的共识,例如病理诊断所需的腺体与子宫内膜基底层的距离。此外,越来越多的诊断基于宫腔镜对子宫内膜缺损、血管过度形成或粘膜下出血性囊肿的观察。没有诊断子宫腺肌病的实验室检查,但如果怀疑大量出血导致贫血,可以测量血红蛋白。
Uterine adenomyosis can be diagnosed using transvaginal ultrasonography (TVUS) and magnetic resonance imaging, with sensitivity in the range of 70% to 80%. Magnetic resonance imaging yields higher specificity than transvaginal ultrasonography (range, 83%-92% vs 74%-81%) and less interobserver variability, and is therefore preferred for interventional treatment planning when not prohibited by cost or lack of availability, such as in low-resource settings. Imaging features frequently seen on ultrasonography include an enlarged uterus, asymmetry of the myometrial thickness, diffusely abnormal / heterogeneously hypoechoic myometrial echotexture, and poorly defined endomyometrial junction. In contrast to fibroids, adenomyosis may have vessels traversing lesions on Doppler ultrasonography findings, while fibroids typically demonstrate peripheral flow. The presence of tiny (1-5mm) anechoic myometrial cysts are specific for diagnosis. On magnetic resonance imaging T2, a hypointense junctional zone can be seen separating the hyperintense endometrium and intermediate-intensity myometrium.
子宫腺肌病可以使用经阴道超声 (TVUS) 和磁共振成像来诊断,其敏感性在 70% 至 80% 之间。磁共振成像产生比经阴道超声检查更高的特异性(范围,83%-92% 对 74%-81%)和更少的观察者间变异性,因此在不受成本或缺乏可用性限制的情况下,作为介入治疗计划的首选,例如在低资源设置。超声检查中常见的影像特征包括子宫增大、子宫肌层厚度不对称、弥漫性异常/异质性低回声子宫肌层回声纹理和子宫内膜交界处界限不清。与肌瘤相反,子宫腺肌病在多普勒超声检查结果中可能有血管穿过病变,而肌瘤通常表现出外周血流。微小(1-5 毫米)无回声子宫肌层囊肿的存在对诊断具有特异性。在磁共振成像 T2 上,可以看到低信号交界区将高信号子宫内膜和中信号子宫内膜分开。
Treatment
治疗
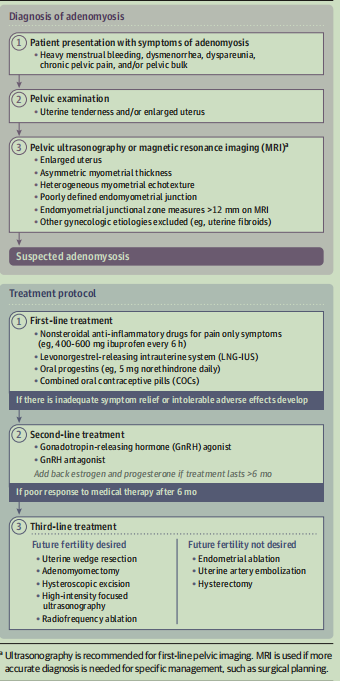
Figure. Suggested Diagnosis and Treatment Algorithm for Adenomyosis
图. 建议的子宫腺肌病诊断和治疗方法
There are no US Food and Drug Administration–approved medical therapies specifically indicated for the treatment of adenomyosis. As a result, adenomyosis is currently managed using modalities developed for contraception and symptoms of heavy menstrual bleeding, dysmenorrhea, and pelvic pain due to other gynecologic conditions (fibroids or endometriosis). Although there are limitedstudies of treatments specifically for adenomyosis, some datacome from trials examining adenomyosis with concomitant gynecologic disorders. Most medical therapies modulate estrogen and progesterone to suppress endometrial proliferation and diminish inflammatory cytokines and prostaglandins.
没有美国食品和药物管理局批准的专门用于治疗子宫腺肌病的药物疗法。因此,子宫腺肌病目前使用针对避孕和其他妇科疾病(子宫肌瘤或子宫内膜异位症)引起的大量月经出血、痛经和盆腔疼痛症状而开发的方式进行管理。尽管专门针对子宫腺肌病的治疗研究有限,但一些数据来自检查子宫腺肌病伴有妇科疾病的试验。大多数医学疗法调节雌激素和孕激素以抑制子宫内膜增殖并减少炎性细胞因子和前列腺素。
When there isa clinical suspicion of adenomyosis, and after other etiologies have been excluded, medical therapy is generally considered before interventional procedures for management ofheavy menstrual bleeding and dysmenorrhea (Figure). The most effective firstline treatment for adenomyosis-relatedpain, bleeding, and associated anemia appears to be the levonorgestrel-releasing intrauterine system. Compared with oral medications, such as progestin-only orcombined oral contraceptive pills, the levonorgestrel-releasing intrauterine system provides a steady state of hormonal medication at a local level while simultaneously providing contraceptive benefit, effectively managing symptoms and avoiding hysterectomy in more than two-thirds of patients. At higher doses than the “mini pill,” the oral progestin norethindrone (5 mg daily) has also been found to be effective for managing adenomyosis-related bleeding and pain. Although it is effective in managing heavy menstrual bleeding and pain, gonadotropin-releasing hormone agonists induce symptoms of hypoestrogenemia, such as hot flashes, which can limit medication adherence andlong-term use. Newer oral gonadotropin-releasing hormone antagonists approved for fibroid and endometriosis-related symptoms may also be effective. Emerging research may also show benefit in the future (eTable in the Supplement). Because of the contraceptive effects of these treatments, fertility outcomes have not been examined, and these medical treatments may not be desirable for those seeking pregnancy.
当临床怀疑子宫腺肌病并排除其他病因后,一般会在介入治疗前考虑药物治疗,以治疗大量月经出血和痛经(图)。子宫腺肌病相关疼痛、出血和相关贫血最有效的一线治疗似乎是释放左炔诺孕酮的宫内节育系统。与仅含孕激素或复方口服避孕药等口服药物相比,释放左炔诺孕酮的宫内节育系统可在局部水平提供稳定的激素药物,同时提供避孕益处、有效控制症状并避免超过三分之二的子宫切除术的患者。在比“迷你药丸”更高的剂量下,口服孕激素炔诺酮(每天 5 毫克)也被发现可有效控制子宫腺肌病相关的出血和疼痛。虽然它对控制大量月经出血和疼痛有效,但促性腺激素释放激素激动剂会引起低雌激素血症的症状,如潮热,这会限制药物依从性和长期使用。被批准用于治疗肌瘤和子宫内膜异位症相关症状的新型口服促性腺激素释放激素拮抗剂也可能有效。新兴研究也可能在未来显示出益处(补充中的电子表格)。由于这些治疗的避孕效果,尚未检查生育结果,并且这些药物治疗可能不适合那些寻求怀孕的人。
Uterine-sparing techniques that have been developed for the management of fibroids are now being applied to the management of adenomyosis. Generally, these options are only considered when patients do not respond tomedical treatment or for fertility-related concerns. Although future fertilityis often desired by women choosing these options, data regarding reproductive outcomes remain limited. Uterine artery embolization is the most well-studied intervention for adenomyosis and effectively decreases heavy menstrual bleeding and dysmenorrhea; however, approximately 25% of patients will undergo subsequent hysterectomy due to persistent symptoms. Pregnancy after uterine artery embolization is not generally recommended based on studies that demonstrated higher rates of obstetric complications, including miscarriage and postpartum hemorrhage. Similarly, endometrial ablation, which seeks to destroy the endometrium, diminishes bleeding and pain, but subsequent pregnancy is not recommended. Excisional procedures, such as adenomyomectomy, uterine wedge resection, and hysteroscopic excision, have shown promise in improving symptoms to varying degrees, with up to 60% of women achieving subsequent pregnancy. These techniques of focal excision of both diffuse and focal adenomyosis are not commonly used, but show promise over more global uterine procedures for women seeking to preserve fertility. For all these interventions, more data are needed regarding the potential benefits on quality of life, fertility, and pregnancy, specifically in patients with adenomyosis rather than mixed groups of patients with symptoms attributable to other etiologies.
为治疗肌瘤而开发的保留子宫技术现在正应用于治疗子宫腺肌病。一般来说,只有当患者对药物治疗或生育相关问题没有反应时,才会考虑这些选择。尽管选择这些选项的女性通常希望未来的生育能力,但有关生殖结果的数据仍然有限。子宫动脉栓塞术是研究最多的子宫腺肌病干预措施,可有效减少大量月经出血和痛经;然而,由于持续的症状,大约 25% 的患者将接受随后的子宫切除术。根据显示产科并发症(包括流产和产后出血)发生率较高的研究,一般不推荐子宫动脉栓塞后怀孕。同样,旨在破坏子宫内膜的子宫内膜消融术可减少出血和疼痛,但不建议随后怀孕。子宫腺肌瘤切除术、子宫楔形切除术和宫腔镜切除术等切除手术已显示出不同程度改善症状的前景,高达 60% 的女性随后怀孕。这些弥漫性和局灶性子宫腺肌病的局灶性切除技术并不常用,但对于寻求保留生育能力的女性来说,在更全面的子宫手术中显示出前景。对于所有这些干预措施,需要更多关于生活质量、生育能力和妊娠的潜在益处的数据,尤其是子宫腺肌病患者,而不是症状可归因于其他病因的混合组患者。
Conclusions
结论
Adenomyosis is more common than generally appreciated and should be included in the differential diagnosis of abnormal uterine bleeding and/or pelvic pain. Several medical therapies and uterinesparing procedures can effectively improve symptoms without need for hysterectomy. Improved clinical awareness is needed to ensure appropriate patient care and to encourage studies to improve the understanding of pathophysiology and drive development of more sensitive noninvasive diagnostics and novel, US Food and Drug Administration–approved treatments.
子宫腺肌病比一般认为的更常见,应包括在异常子宫出血和/或盆腔疼痛的鉴别诊断中。 几种药物疗法和保子宫手术可以有效地改善症状,而无需进行子宫切除术。需要提高临床意识以确保适当的患者护理并鼓励研究以提高对病理生理学的理解并推动开发更敏感的无创诊断和美国食品和药物管理局批准的新型治疗方法。